Smart Q station improves the COVID-19 quarantine workflow

Author(s)
Chiou-Feng LinBiography
Professor Chiou-Feng Lin is the Director of the Department of Microbiology and Immunology in the College of Medicine, Taipei Medical University (TMU). Currently, he serves as Vice Dean of Research & Development and the Director of Immune Monitoring Core at TMU. In 2012, he was awarded a Distinguished Researcher of the Chinese Society of Immunology, Taiwan. His research interests are Infection & Immunity, Oncoimmunology, and Cell Death.
Academy/University/Organization
Taipei Medical University-
TAGS
-
Share this article
You are free to share this article under the Attribution 4.0 International license
- LIFE SCIENCES
- Text & Image
- May 21,2020
To beat infectious diseases, host immunity determines the susceptibility to the pathogens. In the face of infection, herd immunity, created by the complete host immunity, may minimize the outbreak. Fortunately, utilizing biotechnology helps us to avoid lethal infectious diseases by the approaches of pathogen diagnosis, antimicrobial treatment, and preventive vaccination. If wearing a mask is to become unnecessary, strengthening host immunity is the key.
From the end of 2019, a new coronavirus disease 2019 (COVID-19) caused by the novel coronavirus, namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused a pandemic outbreak that is still ongoing. As an emerging infectious disease, as of end-May 2020, SARS-CoV-2 has caused 5 million confirmed cases and over 328 thousand deaths around the world. With a variant case fatality rate ranging from 0.3~6% in the different countries, the strategies, including public prevention, essential diagnosis, and medical practice, generally determine the consequence of the epidemic situation. Until now, the Taiwan government, industry, and research institutes have cooperatively and successfully decreased the outbreak by using technological strategies for public prevention, utilizing rapid methods for further diagnosis, and developing antiviral agents for treatment. The policy of quarantine and isolation is an emerging process for preventing a new outbreak. Due to concern about its imminent return and to take the fight beyond the borders, effective medication and vaccination are necessary for therapeutic and preventive measure, respectively. While critical care medication and antiviral agents are processed for therapy, vaccine development is indispensable to avoid further infection in uninfected/healthy people. Fortunately, several candidates are currently under evaluation and, hopefully, will be available for future vaccination.
Host immunity acts as the critical player for beating COVID-19, but sometimes not. In response to the new SARS-CoV-2 infection, activation of innate immunity generally produces cytokines/chemokines for antiviral defense. Aberrant antiviral interferon response may cause macrophage activation to induce cytokine storm disease. Following immune activation, adaptive immunity confers specific antiviral humoral and cellular responses to neutralize and eradicate the virus as well as the infected cells. Lessons from severe COVID-19 raise the possibilities that aged people and patients with chronic cardiovascular diseases and diabetic metabolic disorders are susceptible to SARS-CoV-2 infection. Many cases, with or without symptoms, show a continued viral infection and have been reported to be infectious carriers. While immunocompromised status is frequently present in those patients with severe disease progression, COVID-19 has also been diagnosed in adult people with rapid progress following 10-day disease onset, suggesting the immune involvement in disease development. The previous studies of SARS-CoV displayed antibody-mediated immunopathogenesis, including antibody-dependent enhancement infection, autoimmune involvement, and antigen-antibody complex-mediated immune activation. Based on the findings, immune-mediated damage is proposed as being vital in the clinical and pathological features of COVID-19.
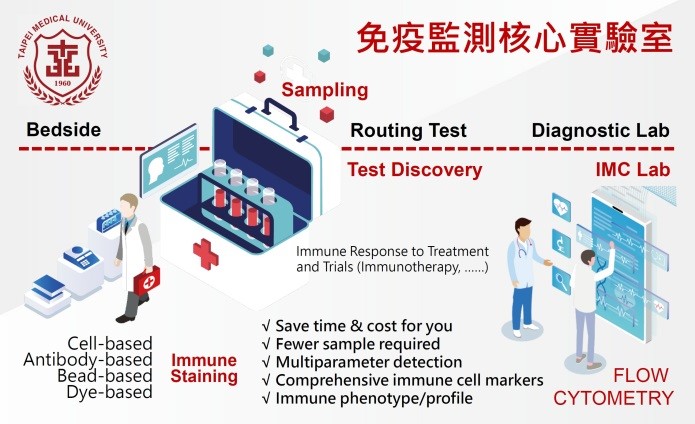
To get a better understanding of the immune status of COVID-19, immune monitoring is therefore suggested. Immune parameters, including the number and the subpopulation of leukocyte/lymphocyte, the expression of cytokine/chemokine, and the generation of immunoglobulins, could be measured by the omics’ approaches in blood samples. As shown by the top universities/institutes around the world, they farsightedly established immune monitoring core facilities for analyzing the immune status and responses, particularly in patients with immune therapy. For the current immune monitoring in COVID-19, aberrant lymphopenia and cytokine response may be used as diagnostic/prognostic biomarkers and are helpful for assisting physicians in treating COVID-19 patients. Under immune monitoring, more immune parameters are identified, and more strategies for manipulating immunity will be beneficial in beating COVID-19.
With the support of Taipei Medical University (TMU) since 2019, the Office of Research and Development creates an Immune Monitoring Core (IMC) to measure the in-depth changes in circulating immune cell populations and immune cell expression in tissues. At the same time, the core laboratory can detect soluble immune parameters, such as cytokines/chemokines and antibodies, as well. By using fewer samples, the time-kinetic evaluation is achievable. The IMC offers state-of-the-art flow cytometry cell analysis and immune cellular function analysis to the intramural research community at TMU and will open for extramural services. In summary, creating an immunogram for identifying the current status in host immunity is suggested as being essential for future medicine related to immunotherapy, immunopathogenesis, and immune modulation.
STAY CONNECTED. SUBSCRIBE TO OUR NEWSLETTER.
Add your information below to receive daily updates.