AI-Enhanced Safety of Prescriptions

Author(s)
Der-Sheng HanBiography
Dr. Han graduated from the College of Medicine, Kaohsiung Medical University and earned his PhD from the Graduate Institute of Clinical Medicine, National Taiwan University (NTU), Taiwan. He is now a Clinical Associate Professor at the Department of Physical Medicine and Rehabilitation, College of Medicine, NTU; and Medical Director in NTU Hospital Bei-Hu Branch.
Academy/University/Organization
National Taiwan UniversityEdited by
Der-Sheng, Han-
TAGS
-
Share this article
You are free to share this article under the Attribution 4.0 International license
- LIFE SCIENCES
- Text & Image
- August 21,2019
The Community and Geriatric Medicine Research Center in National Taiwan University Hospital Bei-Hu Branch is aiming to (1) review the sarcopenia and frailty related literature; (2) find new physical parameters and biomarkers for predicting sarcopenia and frailty; and (3) set up a clinical trial to test the best therapeutic regimen. We have conducted many meta-analyses, cross-sectional studies, and randomized controlled clinical trials focusing on the above-mentioned purposes. We hope to find suitable biomarkers to screen these patients using an easier method. In the long run, we will design the best interventions for the sarcopenic elderly.
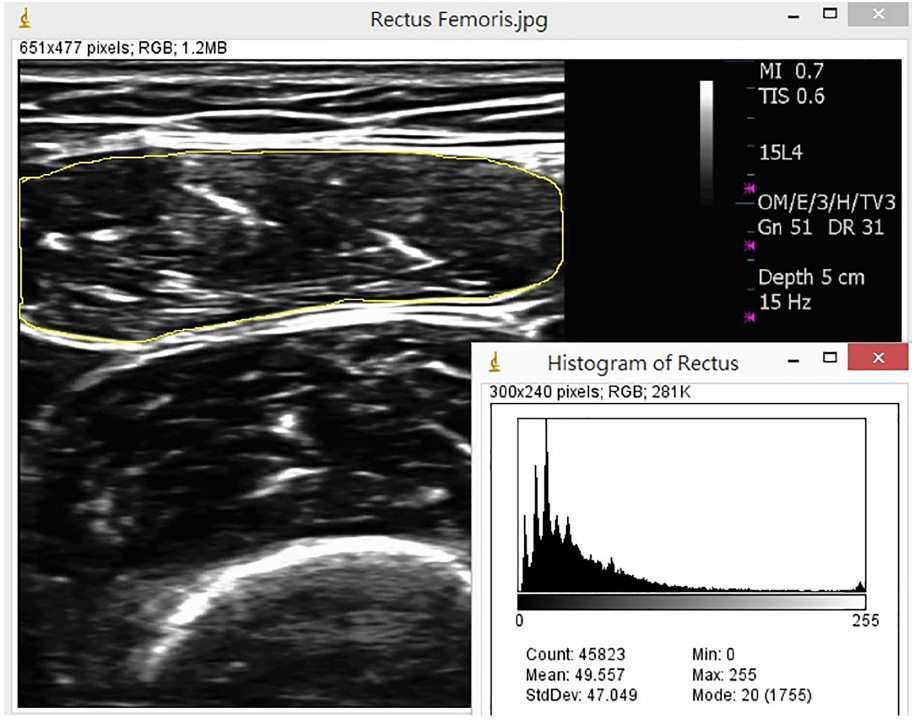
Measurement of muscle mass by ultrasonography
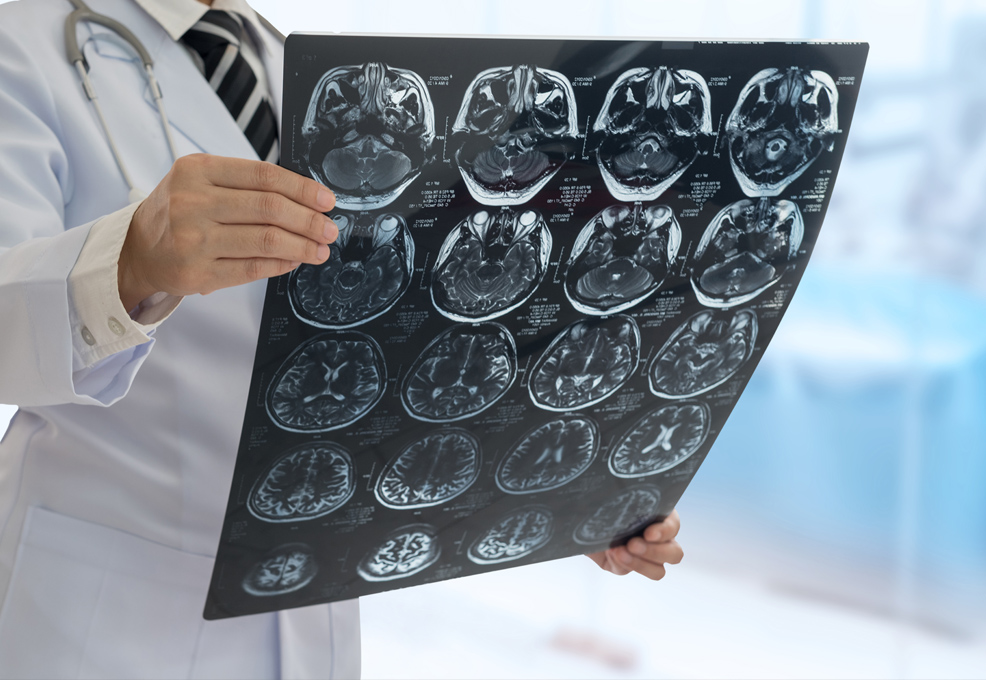
The growth of the aging population has led to increased scientific and medical societies’ interest in the research of aging. Skeletal muscle dysfunction, such as weakness, atrophy or poor coordination is an important risk factor for quality of life and mortality in the elderly. Previous studies have shown that aged people have loss of muscle mass and muscle strength at a rate of 0.64-0.98% and 2.5%-4% per year, respectively. In recent years, there has been growing attention to the sarcopenia, and a consensus on definition has been developed in Europe, Asia and North America. Most of the diagnostic criteria of sarcopenia include muscle strength, physical performance and muscle mass. However, Clark and Manini argued that the loss of muscle mass and strength needs to be defined independently, and so they proposed the term “dynapenia” to describe the age-related loss of muscle strength.
The Community and Geriatric Medicine Research Center, National Taiwan University Hospital Bei-Hu Branch is aiming to (1) review the sarcopenia and frailty-related literature; (2) find new physical parameters and biomarkers for predicting sarcopenia and frailty; and (3) set up a clinical trial to test the best therapeutic regimen.
Aim 1: We have meta-analyzed the association of sarcopenia and its co-morbidities, including cognitive function impairment, depression, hepatocellular carcinoma, and liver cirrhosis.
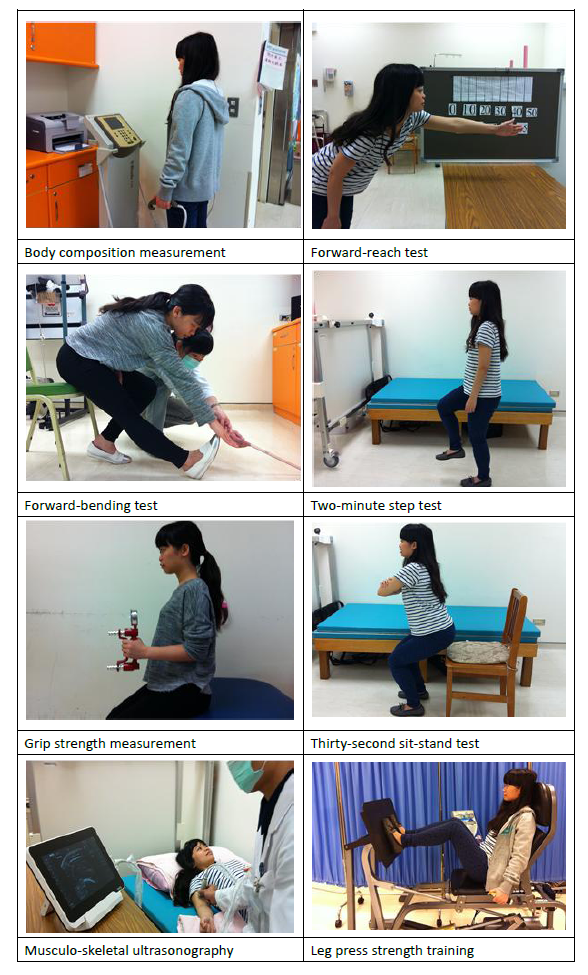
Aim 2: We have established a cohort with 1,000 elderly receiving annual health check-ups. We have employed a new technique, ultrasonography, to evaluate the morphological parameters to predict sarcopenia and frailty. We have found that texture analysis is effective in predicting dynapenia (muscle weakness) without sarcopenia. Besides, we have also suggested that grip strength is good for predicting skeletal muscle mass. It will be quite easy to estimate skeletal muscle mass in the future.
We have also collected blood and urine samples to find biomarkers. The collaborating laboratory is focusing on micro-RNA, extra-cellular vesicles, and metabolomics.
Aim 3: We have conducted a clinical trial recruiting 60 sarcopenic patients to see the effect of combined nutrition supplements and exercise intervention. The intervention is composed of a 12-week strength training program, starting at 40% 1RM, and supplements of calcium, Vitamin D, and branched-chained amino acid on a daily basis. The results showed significant improvements in muscle strength, bone mineral content, and skeletal muscle mass after the combined intervention.
Based on these experiments, we have demonstrated the disease loading of sarcopenia and frailty, and suggest the appropriate resources that should be allocated to this field in the future. Hopefully, we will find suitable biomarkers so as to screen these patients using an easier method. In the long run, we will design the best interventions for the sarcopenic elderly.
STAY CONNECTED. SUBSCRIBE TO OUR NEWSLETTER.
Add your information below to receive daily updates.