What Can AI Technology Do to Help Us Fight against Tuberculosis (TB)?

Author(s)
Yi-Shan TsaiBiography
Dr. Yi-Shan Tsai is an Associate professor of Radiology at National Cheng Kung University and Director of Clinical Innovation and Research Center of NCKU hospital. She is also the Division Chief of Cardiothoracic Imaging of the department of Medical imaging of NCKU Hospital. Dr. Tsai currently leads the development of the medical imaging AI and industry-hospital cooperation of NCKU hospital.
Academy/University/Organization
National Cheng Kung UniversitySource
Third FDA Clearance for Zebra-Med's AI Solution for Brain Bleeds Alerts-
TAGS
-
Share this article
You are free to share this article under the Attribution 4.0 International license
- LIFE SCIENCES
- Text & Image
- November 23,2020
Intracranial hemorrhage results from about 10% to 20% of all strokes and could arise from traumatic injury, ruptured aneurysm, or cancer. The immediate and accurate diagnosis of active intracranial bleeding is necessary for the timely treatment of these patients.
Artificial intelligence (AI) has already had significant impacts on medical imaging. One kind of clinical practice in triage is known as CADt; it is a deep learning-based algorithm acting as the doorkeeper for medical images.
In the past, the radiological technologist started a notification to the doctors of ICH, aortic dissection, and pneumothorax after they finished the exams and checked the image quality. About 10% of ICH patients have delayed alert of more than 10 minutes due to the busy ED environments. Since March of 2020, we have deployed the AI alert model in our daily work for ICH detection based on head CT scans. We achieved an accuracy of 87% and shortened the warning time to less than 2 minutes. The AI alert system automatically read the brain CT scan at ED every 2 minutes and reduced the workload of technologists for notification duty. The performance of AI in clinical practice needs not be superhuman to improve patient care. We should tailor the AI project for the unmet needs and set up a re-training system to face the “real-world data”.
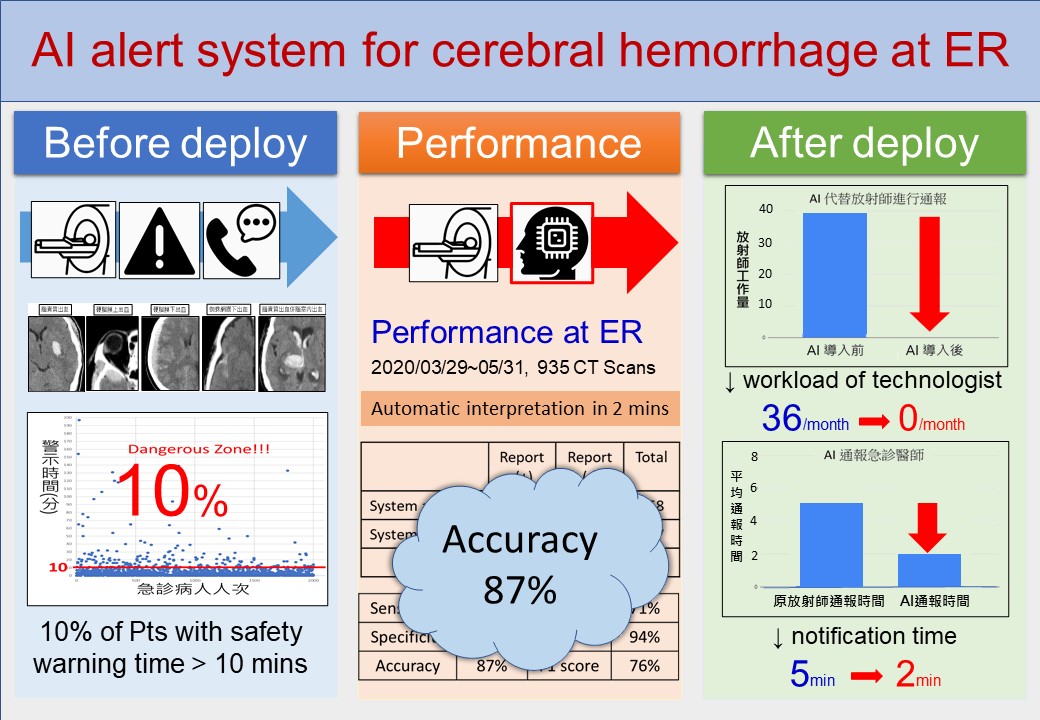
Figure legend: The AI-alert system for ICH at ED has accuracy of 87% and notification time less than 2 minutes after we deploy the system into PACS.
Intracranial hemorrhage results from about 10% to 20% of all strokes and could arise from traumatic injury, ruptured aneurysm, or cancer. The immediate and accurate diagnosis of active intracranial bleeding is necessary for the timely treatment of these patients. ICH, or commonly brain bleed, is fatal and has a high 30-day mortality rate from 35% to 52%. Early detection in the Emergency department (ED) is important to shorten the waiting time of patients with ICHs.
Artificial intelligence (AI) has already had significant impacts on medical imaging. One kind of clinical practice in triage is known as CADt; it is a deep learning-based algorithm acting as the doorkeeper for medical images. The algorithm reads the medical images first and kicks off the notification to the medical staff for early action.
With the development of the smart hospital, we built up AI models collaborating with the Department of Computer Science and Information Engineering (CSIE) for CADt including ICH, aortic dissection, and pneumothorax. All of these three diseases are emergent for ED doctors, and urgent treatment is warranted. In the past, the radiological technologist started a notification to the doctors of ICH, aortic dissection, and pneumothorax after they finished the exams and checked the image quality. About 10% of ICH patients had delayed alert of more than 10 minutes due to the busy ED environments. Since March of 2020, we have deployed the AI alert model in our daily work for ICH detection based on head CT scans. We achieved an accuracy of 87% and shortened the warning time to less than 2 minutes. The AI alert system automatically read the brain CT scan in the ED every 2 minutes, and reduced the workload of technologists regarding their notification duty. So far, we have achieved a good result for ICH detection and further, we want to classify the five subtypes of ICH, intraparenchymal hemorrhage (IPH), epidural hemorrhage (EDH), subdural hemorrhage (SDH), subarachnoid hemorrhage (SAH), and intraventricular hemorrhage (IVH). The preliminary data for the ICH classification model reaches 0%, 96%, 89%, 91% and 98% sensitivity and 100%, 93%, 70%, 81% and 92% specificity for EDH, SDH, SAH, IPH and IVH, respectively. In the future, the research team will include more EDH cases for subtype classification to solve the data imbalance in EDH, which has fewer cases.
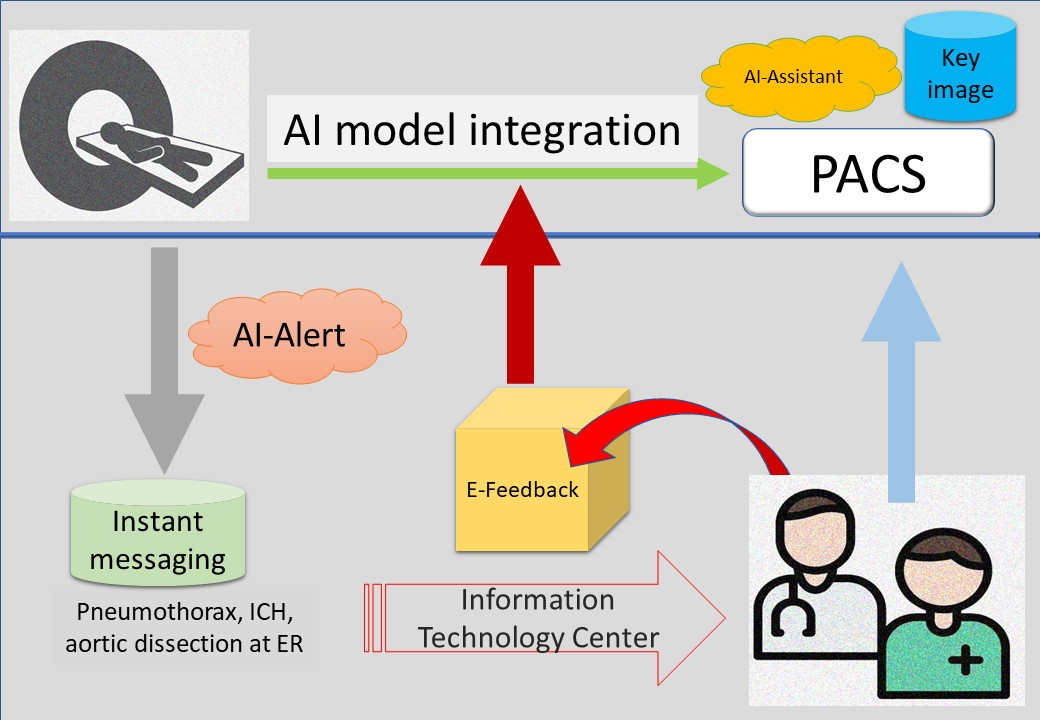
Figure legend: The architecture of medical imaging AI in NCKUH provided AI-alert, AI-assistant and E-feedback systems to improve daily workflow.
Furthermore, we have integrated the AI model with the picture archives communicating system (PACS) acting as an AI assistant tool for anyone who wants the AI model to interpret the medical images for assistant imaging diagnosis. The performance of AI in clinical practice need not be superhuman to improve patient care. If AI can perform at a level better than the lower end of the radiologist performance scale, the patients will benefit. Then we should tailor the AI project for the unmet needs, and set up a re-training system to face the “real-world data.” The intended use of every AI model should be clarified for AI algorithms, research, improving workflow, or commercialization. The process for certification of the AI model is complicated and needs a great deal of verification and validation documentation.

Figure legend: Cooperation of cross-domain teams with good communication is the key for successful smart health.
Cross-domain communication is the first step for successful collaboration in different AI teams with disparate skills and expertise. A good AI model should be built with selfless domain knowledge, and it should be explained simply and recognizably. “Garbage in and garbage out” is the nightmare for smart medicine. High-quality image data and precise labels can provide a guarantee of a useful AI model. The integration of AI and innovative smart healthcare technologies encourages and stimulates greater outstanding information technology in healthcare services to increase efficiency, quality, and healthcare value.
STAY CONNECTED. SUBSCRIBE TO OUR NEWSLETTER.
Add your information below to receive daily updates.